Danielle Kogan Illustrations

Delayed Diagnosis in Women:
Understanding Gender Biases
Meet Charlotte
Stage 4 Endometriosis, 19 yrs To Diagnosis
Charlotte started having symptoms when she was just 8 years old and by the time she was 11, she was diagnosed with ovarian cysts. Further symptoms and cysts got worse over time and when Charlotte saw her doctor she was told that 'she was just someone that had cysts.' One of her long time medical teams mismanaged her care for many years. They potentially thought it was endometriosis or something hormonal but didn't offer any options for pain management except for a variety of birth control options.
She eventually had surgeries in 2014, 2016, 2019, 2020, and 2022. She was finally diagnosed with Stage 4 endometriosis after she traveled to have a Specialist in Portland, Maine to preform surgery for her in 2020. She then in 2022 went to Atlanta, GA for surgery with another specialist who had more experience in thoracic endometriosis. The average length of diagnosis for endometriosis is 7-10 years, and Charlotte's diagnosis took 19 years in total.
When she finally received a diagnosis she stated, "I was relieved because I wasn't crazy and all of the pieces started to come together. Before that there wasn't enough evidence for it to come together. It was also depressing as it took so long. There was a lot of medical trauma and PTSD that came from it."

What Is Delayed Diagnosis?
"A diagnosis that was unintentionally delayed while sufficient information was available earlier."
-(Tudor et al., 2016)

Delayed Diagnosis Timeline
This is a hypothetical representation of a delayed diagnosis timeline.
Each person has a different diagnosis experience.

Symptoms occur

Sees Clinician

Works On Symptom Management
Ugh it isn't getting better...

Sees Clinician Again

Basic Blood Test Done
After 6 Months Sees A Specialist


Multiple Rounds of Blood Tests
Done



Gets Told
Tells Them
"I've had these symptoms for a while."

"Have you tried yoga, therapy, changing your diet?"
Gets Told
Tells Them

"I have tried what you said and it isn't getting better."
"Maybe you have anxiety? Let's run a blood test anyway."

FINALLY
Gets Told
Tells Them

"I think there is something very wrong with me."
"I believe you and we will figure this out together."


Takes 10 Months to Get Imaging Done
Goes Over Results
+
FINALLY Gets A Diagnosis!
Total Time To Diagnosis = 3 years!
It Takes Longer For Women To Get Diagnosed Than Men
Let's Talk About It!
Gender Bias In Medicine
Gender Bias is the preference for one gender over the other and stems from prejudices and stereotypes. Gender bias can also be unconscious, which is known as implicit bias. Researchers note a general trend that doctors do not believe in women’s pain, or that females are “used to internal pain” because of menstruation and childbirth.
Women Are Often Given:
Lower amounts of effective pain medication


More referrals to mental health services
More antidepressant prescriptions

Women Weren’t Legally Required To Be Included In Clinical Trial Research Until 1993....
How does this impact medical training, appointments, diagnosis,
treatment, and innovation?
How Does This Affect Women?

When It Comes To Diagnosis...
There Is Delayed Diagnosis
Due To Gender
The MarketScan Commercial Claims and Encounters (CCAE) dataset includes inpatient, outpatient, procedural, and pharmaceutical claims, representing 80,947,643 women and 77,441,202 men. It’s important to note that stroke and heart attack diagnoses occur more quickly, as their symptoms are typically more outward and easier to identify.
Delayed Diagnosis Primarily Affects Patients With Autoimmune Diseases


20% of people worldwide have autoimmune diseases
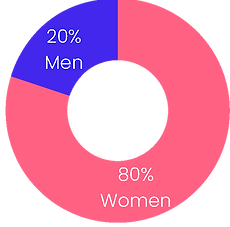
80% of all autoimmune disease
patients are WOMEN
Source: (Angum et al., 2020)
Fibromyalgia

Fibromyalgia has a female preponderance of 3:1.
On average, patients wait 2.3 years and see approximately 3.7 different physicians before receiving a fibromyalgia diagnosis. "This delay is most likely due to the nonspecific clinical features and the lack of clinicians’ comprehension of fibromyalgia."
(Qureshi et al., 2021)
Source: Google
Meet Julie
Fibromyalgia, 6 yrs To Diagnosis
Julie started to have symptoms of fibromyalgia around the age of 12. Their mom, who has lupus and fibromyalgia noticed their symptoms and took Julie to their Primary Care. The male PCP thought they were attention seeking, but didn't want to diagnosis or test them. After fighting with the PCP Julie saw a female PA and got a referral for a pediatric rheumatologist. Unfortunately, the pediatric rheumatologist didn't want to hang a diagnosis on Julie because they were young, so no diagnostic testing was done. The pediatric rheumatologist also put them on hydroxychloroquine.
The medicine managed the pain Julie was experiencing, but Julie didn't get diagnosis of fibromyalgia until around 18 years old after they saw a new female rheumatologist. After the doctor heard the symptoms, they were confused about why Julie hadn’t been diagnosed earlier. They pressed on the fibromyalgia tender points and then quickly said, “You have fibromyalgia. Did anyone tell you?” Julie was shocked that the rheumatologist figured it out just by talking to her.
Getting a diagnosis was was both surreal and freeing after all of that time (after original primary care said she was fine without a diagnosis). "I looked back at all of my symptoms and can say that I wasn't crazy. All the doctors that actually diagnosed me were female. I will not see male doctors anymore. Hopefully things will change, but not without us making it happen. There's hope, I think."

Not All Stories Are Like This Though
A Story of Hope


"My lupus diagnosis was very shocking because there is part of you that suspects that something is causing all these things that are slightly abnormal. My symptoms were worse versions of what normal people experience (fevers, mouth ulcers, etc). I thought what I was experiencing was just all in my head. When it ends up actually being something, everything aligns."
"I was lucky as most women get diagnosed in the their 30s and 40s. I have a incredible doctor that was vigilant... my diagnosis process could have gone a lot differently. This shows the power of a physician that does their job properly."
-Anonymous, 15 years of symptoms, 1 month to diagnosis after seeing physician
Lupus

90% of people diagnosed with lupus are WOMEN and on average it takes nearly 6 years from first symptom to diagnosis.
"63% of people with lupus surveyed report being incorrectly diagnosed. Of those reporting incorrect diagnosis, 55% report seeing four or more different healthcare providers for their lupus symptoms before being accurately diagnosed,"
(Lupus Foundation of America, 2021).
Gender Bias Not Only Affects Diagnosis; It’s Also Killing Women
Morbidity Is Linked To Gender Bias
HOW TO READ THIS CHART:
Gender Concordance is when a patient and physician have the same gender. This chart models the effect of gender concordance on healthcare outcomes particularly patient survival. It was found that female patients with a male physician have a decreased survival rate (-0.01%) compared to female patients that had a female physician (0.03%).
Coefficient estimates and Ordinary Least Squares (OLS) are used to evaluate the correlation of multiple variables.
Doctors are more likely to label symptoms in women as “atypical” compared to those in men. Women often don’t present with “classic” heart attack symptoms and are therefore less likely to receive timely treatment. According to The American Heart Association, this gap exists because diagnostic criteria are largely based on male physiology. Data also show that women having a heart attack are more likely to die when treated by a male doctor, an effect that decreases as male physicians gain more experience working with female patients and colleagues.
Systemic Solutions To Delayed Diagnoses

Create a more rigorous system for communicating abnormal test results to patients.

Implement dedicated hotlines to connect primary care with specialists for timely case discussions.

Improve primary care clinician training in key clinical areas and implicit bias.
Foster improved, transparent communication between clinicians and with patients.
Systemic changes are needed to achieve healthcare equity FOR ALL, not only gender equity.
Source: (Matthew, 2018), (Blach, 2024)
Resources For Patient Advocacy
You can be your own best advocate!
Disease Specific Resources:
Citations
Sun, T. Y., Hardin, J., Nieva, H. R., Natarajan, K., Cheng, R. F., Ryan, P., & Elhadad, N. (2023). Large-scale characterization of gender differences in diagnosis prevalence and time to diagnosis. medRxiv : the preprint server for health sciences, 2023.10.12.23296976. https://doi.org/10.1101/2023.10.12.23296976
Tudor Car, L., Papachristou, N., Bull, A., Majeed, A., Gallagher, J., El-Khatib, M., Aylin, P., Rudan, I., Atun, R., Car, J., & Vincent, C. (2016). Clinician-identified problems and solutions for delayed diagnosis in primary care: a PRIORITIZE study. BMC family practice, 17(1), 131. https://doi.org/10.1186/s12875-016-0530-z
Whitacre CC. Sex differences in autoimmune disease. Nat Immunol. 2001;2(9):777-780. https://doi.org/10.1038/ni0901-777
Qureshi, A. G., Jha, S. K., Iskander, J., Avanthika, C., Jhaveri, S., Patel, V. H., Rasagna Potini, B., & Talha Azam, A. (2021). Diagnostic Challenges and Management of Fibromyalgia. Cureus, 13(10), e18692. https://doi.org/10.7759/cureus.18692
Lupus facts and statistics. Lupus Foundation of America. (2021). https://www.lupus.org/resources/lupus-facts-and-statistics#:~:text=Lupus%20is%20known%20as%20%22the,first%20notice%20their%20lupus%20symptoms.
Biggers, A. (2021). Gender bias in medical diagnosis: Facts, causes, and impact. Medical News Today. https://www.medicalnewstoday.com/articles/gender-bias-in-medical-diagnosis#how-does-it-affect-diagnosis
Angum, F., Khan, T., Kaler, J., Siddiqui, L., & Hussain, A. (2020). The Prevalence of Autoimmune Disorders in Women: A Narrative Review. Cureus, 12(5), e8094. https://doi.org/10.7759/cureus.8094
Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115(34):8569-8574. https://doi.org/10.1073/pnas.1800097115
Matthew, D. B. (2018). Just medicine: A cure for racial inequality in American Health Care. New York University Press.
Merone, L., Tsey, K., Russell, D., Daltry, A., & Nagle, C. (2022). Self-Reported Time to Diagnosis and Proportions of Rediagnosis in Female Patients with Chronic Conditions in Australia: A Cross-sectional Survey. Women's health reports (New Rochelle, N.Y.), 3(1), 749–758. https://doi.org/10.1089/whr.2022.0040
Sloan, M., Harwood, R., Sutton, S., D’Cruz, D., Howard, P., Wincup, C., Brimicombe, J., & Gordon, C. (2020). Medically explained symptoms: A mixed methods study of diagnostic, symptom and support experiences of patients with lupus and related systemic autoimmune diseases. OUP Academic. https://academic.oup.com/rheumap/article/4/1/rkaa006/5758274#supplementary-data
Mayo Foundation for Medical Education and Research. (2024). Medical Diseases & Conditions. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions
Balch, B. (2024). Why we know so little about women’s health. AAMC. https://www.aamc.org/news/why-we-know-so-little-about-women-s-health#:~:text=Before%201993%2C%20women%20were%20rarely,and%20devices%20work%20for%20women.





%20copy.png)





